Improving Blood Culture Contamination in an Adult Emergency Department Utilizing Sideline Technology
Lesly Evert, BSN, RN, CEN, EMT-P and Tina Nielson, RN, MS, CEN, ACNS-BC, APNP
Froedtert Hospital, Milwaukee, WI
Emergency Nursing 2025
Purpose
The purpose of this project was to decrease the BCC rate in an Academic Medical Center and expand knowledge about adherence to best practice to positively affect patient outcomes.
Problem
Emergency Department blood culture contaminations rate reported at 6%.
Blood culture contamination (BCC) can lead to:
- Increased patient length of stay
- Cost increase of $6026 per patient stay
- Cost $4538 per false positive specimen
- Misdiagnosis or unintentional harm
- Increase risk for hospital-acquired infections (HAI) and impair hospital efforts to reduce HAI
- False Positive blood cultures impair antibiotic optimization
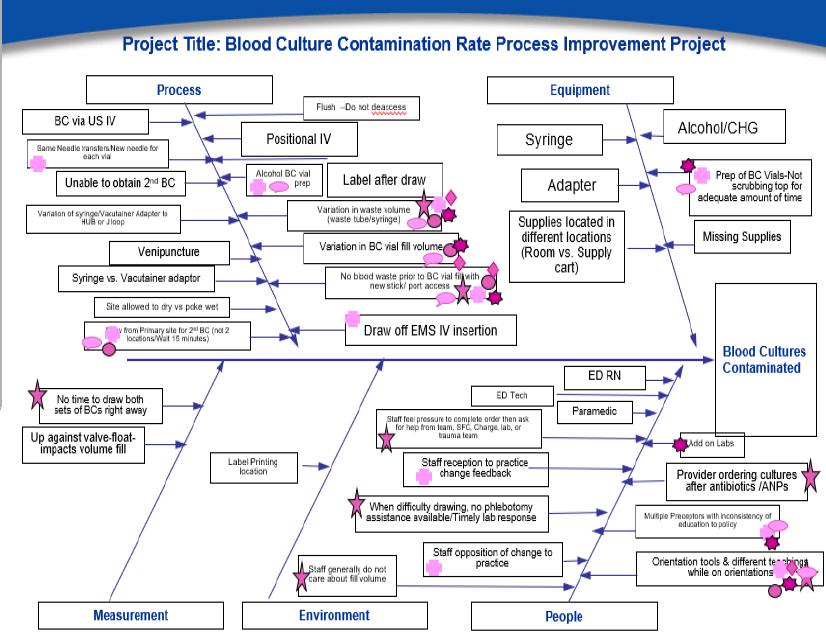
Gap Analysis:
- Educational inconsistency and variation in blood culture collection
- Inconsistent waste prior to specimen collection
- Blood Culture fill volume variation
Clinical Question
In an adult Emergency Department, does skin prep and wasting blood before specimen collection using a specimen diversion device (ISDD) reduce contamination rates of blood cultures to < 1%?
Setting and Sample
- Emergency Department in the Midwest, Level I, Academic Medical Center
- ED staff collecting blood culture specimens
Design
An evidenced-based practice project utilizing the John Hopkins-Evidence Based Practice Model
Methods
Educational Strategies:
- Newsletter, videos, skills fair, presentations, peer observation, poster and signage
- In-person Initial Specimen Diversion Device (ISDD) training
- Process feedback via direct communication and leader rounding
- Standardized tools
Learning Objectives:
- Improve skin preparation, sample waste, and optimal fill volume for blood culture collection
- Create a consistent practice of blood culture specimen collection
- Decreased BCC rates
Data collected:
- Timeframe: July 2023-August 2024
- Blood culture specimen collection observation
- BCC case review
- BCC rates
- ISDD utilization (device inventory)
Results
Findings/Outcomes
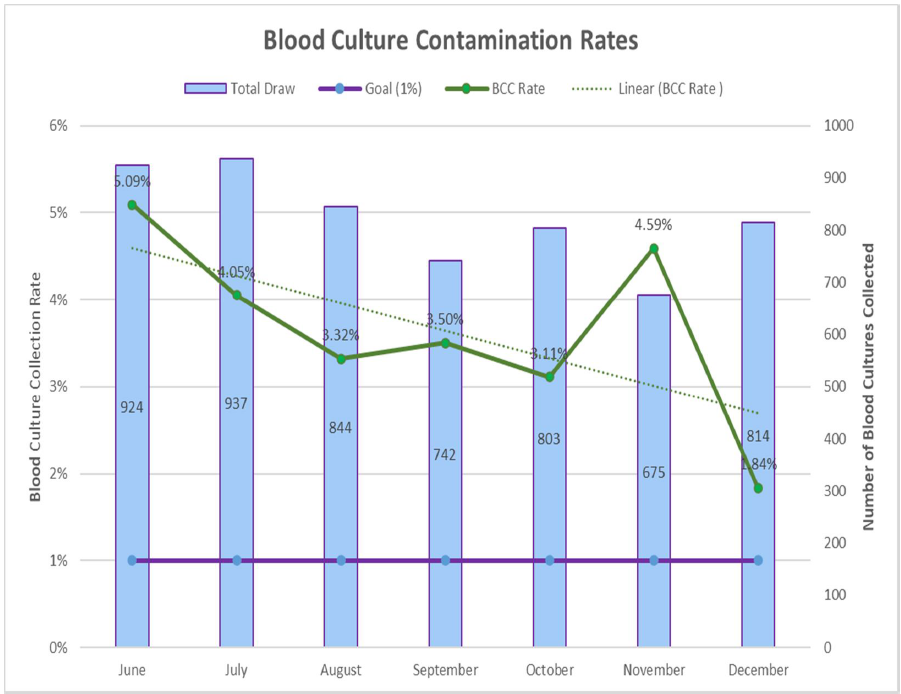
Results
- 100% of observations demonstrated improved consistent blood culture collection practice
- BCC rates decreased from 6% to 2.9% during the initial pilot (52% improvement)
- Lowest BCC rate during project was 0.9%
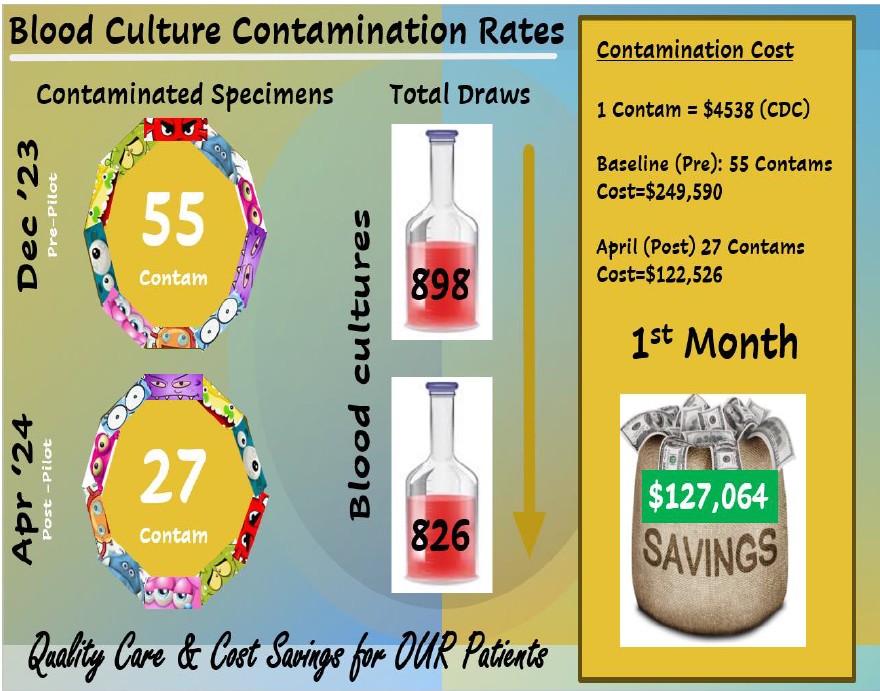
- Projected annual cost savings:
- Decreased in ~40 false positive per month:~$2.2 M
- Decreased in patient length of stay (2 days):~$2.9M
- Total Savings of ~5.1M annually
Conclusions
This project demonstrated that a multimodal approach improved BCC rates. Methods include:
- Reinforcement of the crucial role staff have in blood culture collection and the impact it has on improving patient care outcomes
- Observations and feedback enhanced accountability
- Champion support by peer and leader rounding
- Engage stakeholders in device evaluation to promote practice sustainability
A limitation of the project was we were unable to account for compliance with ISDD utilization.
Implications for Practice
Standardized education and implementation of ISDD for waste diversion should be initiated for consistent blood culture collection.
Acknowledgement
ED Shared Governance, nursing staff, leadership and lab for their support and ongoing focus to providing quality patient care
For additional information please contact:
Lesly Evert, BSN, RN, CEN, EMT-P
Emergency Department, Froedtert Hospital
Lesly.Evert@froedtert.com
Read full text here
